✍️ Authored by the ACSPR Team | ACSPR (Humanitarian Response & Resilience)
📌 Shaping Africa’s Future with Evidence, Equity, and Innovation for Impact
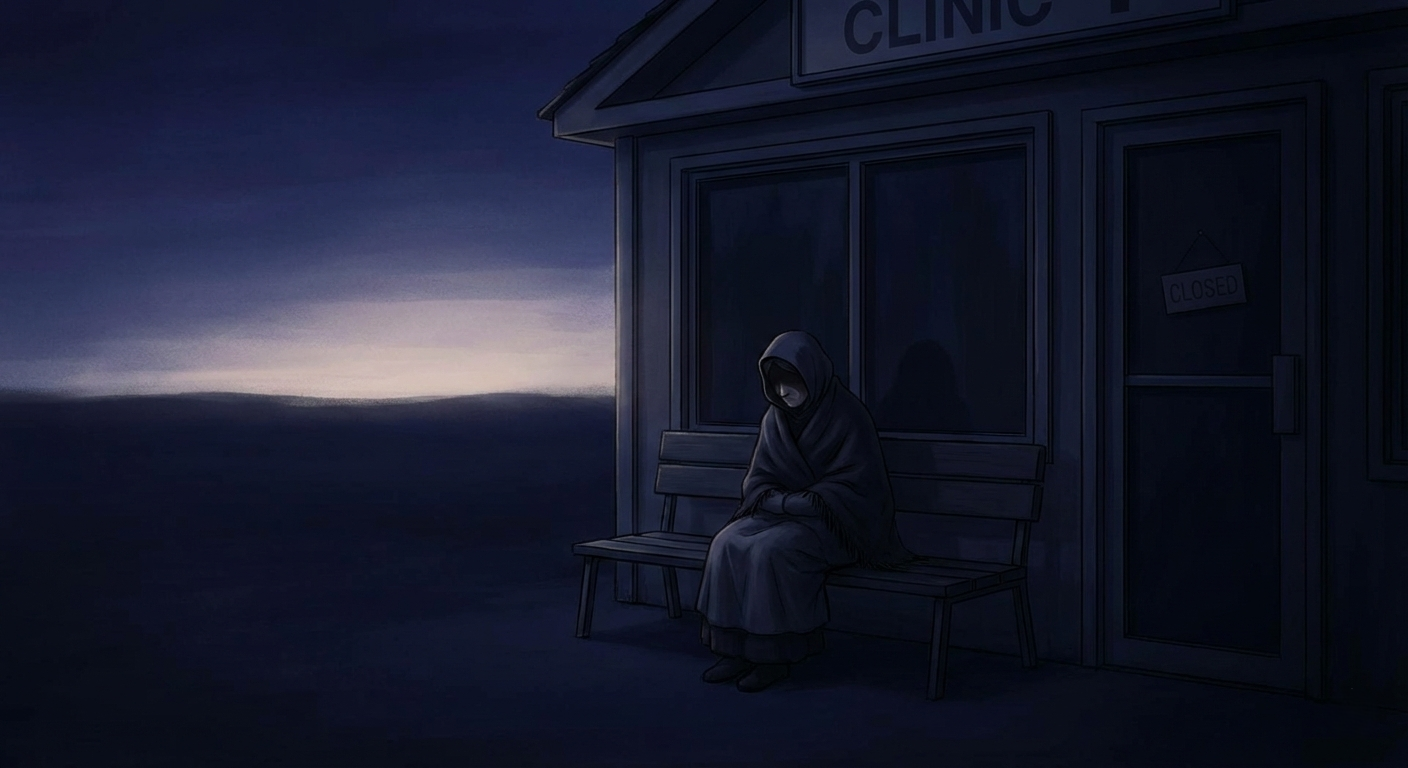
For thousands of adolescent girls and young women living in humanitarian settlements in Uganda, sexual and reproductive health is not simply about services. It is about power, privacy, survival, and dignity.
📌 Shaping Africa’s Future with Evidence, Equity, and Innovation for Impact
For thousands of adolescent girls and young women living in humanitarian settlements in Uganda, sexual and reproductive health is not simply about services. It is about power, privacy, survival, and dignity.
A new quantitative report, “The Sexual and Reproductive Health Needs and Challenges of Adolescent Girls and Young Women in Humanitarian Settings in Nigeria and Uganda,” sheds light on what life looks like for girls aged 15–24 in Nakivale Refugee Settlement (Isingiro District). The findings reveal a system where services may exist, but access, awareness, and autonomy remain deeply constrained.
The Humanitarian Context: A Generation at Risk
By the end of 2021, about 89 million people were forcibly displaced globally. Many are women, girls, and young people facing heightened risks related to SRHR vulnerabilities and gender-based violence.
In Uganda, Nakivale Refugee Settlement hosts nearly 146,000 refugees across almost 40,000 households. Adolescent girls and young women represent a significant share of this population - navigating displacement during one of the most critical stages of physical and social development.
Humanitarian settings intensify existing vulnerabilities, increasing risks of early pregnancy, unsafe abortion, intimate partner violence, and exploitation.
SRHR Service Use: Available, But Not Fully Accessible
The study surveyed 461 adolescent girls and young women aged 15–24 in Nakivale.
Key findings include:
● 63% of sexually active young women reported using some form of contraception.
● Yet only 26% reported using SRHR services within the settlement.
This gap suggests a troubling reality: even where contraception is being used, many young women may not be accessing comprehensive SRHR care.
The report points to three major drivers of low service utilization:
● Low decision-making power
● Stigma surrounding SRHR
● Limited awareness of available services
The Invisible Barriers
Limited decision-making power
Reduced autonomy within relationships significantly affects contraceptive use and access to care. Decision-making power often shaped by early marriage and limited education influences whether a girl can seek services at all. When girls cannot independently decide about contraception or clinic visits, services become theoretical rather than practical.
Stigma and confidentiality concerns
Fear of being seen at clinics remains a major barrier. Confidentiality concerns including worries about consent requirements discourage many from seeking care. Without private waiting areas, youth-friendly providers, and clear confidentiality protocols, many young women choose silence.
Lack of awareness
Among sexually active women not using contraception, lack of information was a key reason. Even in Uganda where awareness levels were higher than in Nigeria, 21% of those who had not accessed SRHR care in the settlement reported this was due to lack of information. Information gaps remain especially critical for unmarried girls who may face additional stigma.
Living Conditions Compound the Crisis
SRHR cannot be separated from daily survival realities.
● 91% reported not having sufficient food.
● 84% said food rations were insufficient for their family’s needs.
● Only about one-quarter had access to income.
When food security and income are unstable, healthcare especially preventive SRHR services often becomes secondary.
Menstrual hygiene management also varies, with reliance on reusable and disposable pads depending on availability - underscoring the need for integrated SRHR and dignity kit programming.
Gender-Based Violence: Underreported and Under-addressed
Humanitarian settings heighten exposure to intimate partner violence and other forms of GBV, yet help-seeking remains low. Few survivors report to police or legal actors; many turn instead to informal networks such as friends, neighbours, or religious leaders highlighting a trust gap between survivors and formal response systems.
What Needs to Change?
● Conduct further research with service providers, NGOs, and families to understand drivers of stigma
● Provide gender norms training and SRHR education for men and elders to reduce social barriers
● Strengthen confidentiality protections and remove harmful consent barriers
● Increase awareness campaigns on available services
● Integrate IPV/GBV screening and referral pathways within SRHR services
SRHR services must move beyond availability to accessibility privacy, youth-friendliness, and trust.
From Survival to Dignity
For adolescent girls and young women in Uganda’s refugee settlements, SRHR is not only about contraception or clinic visits. It is about whether she can decide, whether she can ask questions, and whether she can seek care without fear.
Humanitarian response must treat SRHR not as an optional add-on, but as a core life-saving service because displacement should not mean the loss of choice.